en
names in breadcrumbs


C. neoformansis a possibly pathogenic fungal microorganism. They produce prominent capsules which aid in the evasion of host defenses. C. neoformanscommonly infects the tissue of the respiratory system, but can manifest as a fungal encephalitis as well. It's method of entry is commonly via the respiratory route.
The ability to grow at 37 C distinguishes it from other Cryptococcus species however a few temperature sensitive mutants are possible.
C. neoformans var. gattii is only found on Eucalyptus camaldulensis. Some research considers it to be a distinct species.
Canavanine-glycine-bromthymol blue (CGB) medium can be used to distinguish from var. gattii. C. neoformans var. gattii will produce a blue color on the media.
In histopathology sections var. gattii produces more elongated, oval, or elliptical cells where var. neoformans produces more strictly globose cells.
Filobasidiella neoformans var. bacillispora produces smooth, rod-shaped basidiospores and no haustrioid hyphae.
C. neoformans var. grubii cannot utilize thymine. Also significant genetic differences using DNA fingerprinting have also been reported. (Franzot et. al.,1999)
It is ubiquitous. It is often a laboratory contaminant.
Colonies are white to dark cream colored, smooth, mucoid, glistening to dull and generally grow slower than Candida. The degree of mucoidness is proportional to the amount of polysaccharide capsule that the fungus produces. Colonies that have small capsules may be wrinkled and granular in appearance. They grow well at 25 C and 37 C. Temperatures above 37 C slow the fungus growth. When grown on media containing diphenolic compounds colonies are brown to black in color.
Microscopically yeast cells are globose to ovoid, thick-walled, budding cells that do not produce hyphae or pseudophyphae. Polysaccharide capsules can be seen using India Ink preparation. The capsules can be up to twice the radius of the yeast cell.
This genus includes four serotypes A-D. Until recently serotypes A and D were included in Cryptococcus neoformans var. neoformans and serotypes B and C were included in Cryprococcus neoformans var. gattii. However a new variety, var. grubii has been proposed to contain serotype A.
The teleomorph of Cryptococcus neoformans var. neoformans is Filobasidiella neoformans var. neoformans and can be induced by placing two isolates of serotype D of opposite mating types in V-8 juice agar. The yeast cells will conjugate and produce long hyphae with clamp connections, haustria-like hyphae, and dolipore (nuclei cannot pass through) septa.
Terminal basidia form from the hyphae in about three weeks. The basidia are slender, subglobose to club-shaped, and non-septate.
Basidiospores are sessile, slightly rough, oval, pyriform, cylindrical to elliptical, uninucleate, and produced in chains by basipetal budding at the apex of the basidia, i.e., at the base of the chain.

a | The fungal polysaccharide capsule is produced in response to environmental cues, in this case after five days in the rabbit central nervous system. India ink (black) is excluded from the fungus by the capsule. b | The fungus produces melanin in the presence of diphenolic molecules (such as L-DOPA) to turn brown or black, in contrast to the common human pathogenic yeast Candida albicans, which forms white colonies on this medium. c | The fungus is a basidiomycete, able to produce filaments when two opposite mating partners (KN99 MAT and Bt63 MATa) are co-cultured, producing four chains of haploid basidiospores from a basidium (inset).
Reprinted by permission from Macmillan Publishers Ltd: [Nature Reviews Microbiology 3, 753-764] (Idnurm, 2005), copyright (2005)
It is an opportunistic pathogen in humans.
It has been isolated from soil, plants, fruit, milk, skin, feces of people in normal health, and most notoriously pigeon dung. It has also been isolated from many other bird droppings as well including chickens, canaries, parrots, and swallows. Initially it was thought that pigeons were carriers of the disease however it has been seen that there is not an increase in disease in areas with a lot of pigeon dung. Pigeons do not become infected with the disease because their body temperature is too high and the yeast simply pass through their gut and grows in their dung.
It may be more useful to find the ecological niche of the teleomorph because basidiospores are dry, readily airborne, and small enough to fit inside the alveoli of the lungs.
It must be distinguished from all other clinically important yeasts.
An India Ink stain can be used to see capsule production.
The absence of hyphae or pseudohyphae distinguishes it from Candida albicans.
The lack of arthroconidia distinguishes it from Trichosporon and Geotrichum.
It cannot ferment sugars.
The ability to assimilate insitol distinguishes it from another common basidiomycetous yeast, Rhodotorula.
The ability to assimilate insitol and produce urease distinguishes it from Candida glabrata.
The ability to produce melanin on media containing diphenolic compounds can also be a distinguishing factor.
Latex agglutination tests can also be used to identify the serotype.
Commercially available DNA probes are useful to laboratories that need rapid and accurate identification of Blastomyces dermatitidis, Histoplasma capsulatum, Coccidioides immitis, and C. neoformans.
C. neoformans is an opportunistic pathogen that commonly causes a disease called cryptococcosis in AIDS patients or people who are taking corticosteroids, have organ transplants, or are on chemotherapy drugs.
Cryptococcosis or Busse-Buschke disease is acquired by inhalation of the yeast cells or basidiospores into the lungs. The infection is subacute or chronic. The chronic form is most commonly found in the brain causing meningoencephalitis. This form is the most common among AIDS patients. The disease can also occur in the lungs, skin, bones, joints, eyes, myocardium, urinary tract, and prostate gland (see image).

Histology of the biopsy specimen of the prostate. (a) Granulomatous lesion of the prostate (HE, 200). (b) High magnification of the granuloma. Small round organisms are scattered in granulomas (HE, 400). © Grocott’s methenamine silver demonstrates numerous yeast-form pathogens in the granulomatous lesion. (d) The pathogen is clearly stained with periodic acid-Schiff with diastase treatment. (e) Fontana-Masson stain demonstrates melanin in the cell wall. (f) The mucoid capsule of the pathogen is stained with mucicarmine.
Reprinted by permission from Macmillan Publishers Ltd: [Nature Reviews Microbiology 3, 753-764] (Idnurm, 2005), copyright (2005)
Meningoencephalitis is the most deadly form of this disease. It can progress rapidly and suddenely induce a coma. Tissue that is in contact with the yeast becomes compressed from the fungus growth but is not necrotic, hemorrhagic, or engorged with blood.
Pulmonary cryptococcosis can be misdiagnosed as Tuberculosis. Treatment with an antibiotic causes the fungal infection to worsen. Upon x-ray fungus can be seen forming extensive lesions in the lungs.
Infection of the skin is either a milder form of the disease or is a sign of a more extensive infection somewhere else in the body. Skin infections show up as small papules and either resolve one their own or are surgically removed.
C. neoformans has some virulence factors that make it a successful pathogen. The ability to grow at body temperature give it the ability to become a pathogen. The polysaccharide capsule protects it from phagocytosis. The production of melanin from diphenolic compounds is also considered a virulence factor because the melanin accumulates in the cell wall and protects the yeast from free radicals produced by host cells.
Treatment for cryptococcosis is Amphoteracin B followed by 5-Fluorocytosine. It is not easily cured in immunosuppressed patients.
Cryptococcus neoformans is an encapsulated yeast[1] belonging to the class Tremellomycetes and an obligate aerobe[2] that can live in both plants and animals. Its teleomorph is a filamentous fungus, formerly referred to Filobasidiella neoformans. In its yeast state, it is often found in bird excrement. Cryptococcus neoformans can cause disease in apparently immunocompetent, as well as immunocompromised, hosts.[1][3]
Cryptococcus neoformans has undergone numerous nomenclature revisions since its first description in 1895. It formerly contained two varieties: C. neoformans var. neoformans and C. neoformans var. grubii. A third variety, C. neoformans var. gattii, was later defined as a distinct species, Cryptococcus gattii. The most recent classification system divides these varieties into seven species.[4] C. neoformans refers to C. neoformans var. grubii. A new species name, Cryptococcus deneoformans, is used for the former C. neoformans var. neoformans. C. gattii is divided into five species.
The teleomorph was first described in 1975 by K.J. Kwon-Chung, who obtained cultures of Filobasidiella neoformans by crossing strains of the yeast C. neoformans. She was able to observe basidia similar to those of the genus Filobasidium, hence the name Filobasidiella for the new genus.[5] Following changes to the International Code of Nomenclature for algae, fungi, and plants, the practice of giving different names to teleomorph and anamorph forms of the same fungus was discontinued, meaning that Filobasidiella neoformans became a synonym of the earlier name Cryptococcus neoformans.
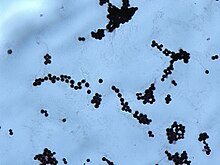
Cryptococcus neoformans typically grows as a yeast (unicellular) and replicates by budding. It makes hyphae during mating, and eventually creates basidiospores at the end of the hyphae before producing spores. Under host-relevant conditions, including low glucose, serum, 5% carbon dioxide, and low iron, among others, the cells produce a characteristic polysaccharide capsule.[6] The recognition of C. neoformans in Gram-stained smears of purulent exudates may be hampered by the presence of the large gelatinous capsule which apparently prevents definitive staining of the yeast-like cells. In such stained preparations, it may appear either as round cells with Gram-positive granular inclusions impressed upon a pale lavender cytoplasmic background or as Gram-negative lipoid bodies.[7] When grown as a yeast, C. neoformans has a prominent capsule composed mostly of polysaccharides. Under the microscope, the India ink stain is used for easy visualization of the capsule in cerebral spinal fluid.[8] The particles of ink pigment do not enter the capsule that surrounds the spherical yeast cell, resulting in a zone of clearance or "halo" around the cells. This allows for quick and easy identification of C. neoformans. Unusual morphological forms are rarely seen.[9] For identification in tissue, mucicarmine stain provides specific staining of polysaccharide cell wall in C. neoformans. Cryptococcal antigen from cerebrospinal fluid is thought to be the best test for diagnosis of cryptococcal meningitis in terms of sensitivity, though it might be unreliable in HIV-positive patients.[10]
The first genome sequence for a strain of C. neoformans (var. neoformans; now C. deneoformans) was published in 2005.[11]
Studies suggest that colonies of C. neoformans and related fungi growing on the ruins of the melted down reactor of the Chernobyl nuclear power plant may be able to use the energy of radiation for "radiotrophic" growth.[12]
Infection with C. neoformans is termed cryptococcosis. Most infections with C. neoformans occur in the lungs.[13] However, fungal meningitis and encephalitis, especially as a secondary infection for AIDS patients, are often caused by C. neoformans, making it a particularly dangerous fungus. Infections with this fungus are rare in people with fully functioning immune systems, hence C. neoformans is often referred to as an opportunistic pathogen.[1] It is a facultative intracellular pathogen[14] that can utilize host phagocytes to spread within the body.[15][16] Cryptococcus neoformans was the first intracellular pathogen for which the non-lytic escape process termed vomocytosis was observed.[17][18] It has been speculated that this ability to manipulate host cells results from environmental selective pressure by amoebae, a hypothesis first proposed by Arturo Casadevall under the term "accidental virulence".[19]
In human infection, C. neoformans is spread by inhalation of aerosolized basidiospores, and can disseminate to the central nervous system, where it can cause meningoencephalitis.[20] In the lungs, C. neoformans cells are phagocytosed by alveolar macrophages.[21] Macrophages produce oxidative and nitrosative agents, creating a hostile environment, to kill invading pathogens.[22] However, some C. neoformans cells can survive intracellularly in macrophages.[21] Intracellular survival appears to be the basis for latency, disseminated disease, and resistance to eradication by antifungal agents. One mechanism by which C. neoformans survives the hostile intracellular environment of the macrophage involves upregulation of expression of genes involved in responses to oxidative stress.[21]
Traversal of the blood–brain barrier by C. neoformans plays a key role in meningitis pathogenesis.[23] However, precise mechanisms by which it passes the blood-brain barrier are still unknown; one recent study in rats suggested an important role of secreted serine proteases.[24] The metalloprotease Mpr1 has been demonstrated to be critical in blood-brain barrier penetration.[25]
Meiosis (sexual reproduction), another possible survival factor for intracellular C. neoformans
The vast majority of environmental and clinical isolates of C. neoformans are mating type alpha. Filaments of mating type alpha have haploid nuclei ordinarily, but these can undergo a process of diploidization (perhaps by endoduplication or stimulated nuclear fusion) to form diploid cells termed blastospores. The diploid nuclei of blastospores are able to undergo meiosis, including recombination, to form haploid basidiospores that can then be dispersed.[26] This process is referred to as monokaryotic fruiting. Required for this process is a gene designated dmc1, a conserved homologue of genes recA in bacteria, and rad51 in eukaryotes (see articles recA and rad51). Dmc1 mediates homologous chromosome pairing during meiosis and repair of double-strand breaks in DNA.[27] One benefit of meiosis in C. neoformans could be to promote DNA repair in the DNA-damaging environment caused by the oxidative and nitrosative agents produced in macrophages.[26] Thus, C. neoformans can undergo a meiotic process, monokaryotic fruiting, that may promote recombinational repair in the oxidative, DNA-damaging environment of the host macrophage, and this may contribute to its virulence.
Infection starts in lungs, disseminates via blood to meninges and then to other parts of the body. Capsule inhibits phagocytosis. Can cause a systemic infection, including fatal meningitis known as meningoencephalitis in normal, diabetic and immunocompromised hosts. The infection from C. neoformans in the brain can be fatal if untreated. CNS (central nervous system) infection may also be present as a brain abscess known as cryptococcomas, subdural effusion, dementia, isolated cranial nerve lesion, spinal cord lesion, and ischemic stroke. If cryptococcal meningitis occurs, mortality rate is between 10 and 30%.[28]
Cryptococcosis that does not affect the central nervous system can be treated with fluconazole alone.
Cryptococcal meningitis should be treated for two weeks with intravenous amphotericin B 0.7–1.0 mg/kg/day and oral flucytosine 100 mg/kg/day (or intravenous flucytosine 75 mg/kg/day if the patient is unable to swallow). This should then be followed by oral fluconazole 400–800 mg daily for ten weeks[29] and then 200 mg daily for at least one year and until the patient's CD4 count is above 200 cells/mcl.[30][31] Flucytosine is a generic, off-patent medicine. However, a market failure exists, with a two-week cost of flucytosine therapy being about $10,000. As a result, flucytosine is currently universally unavailable in low- and middle-income countries. In 1970, flucytosine was available in Africa.[32] The dose of 200 mg/kg/day for flucytosine is not more effective, is associated with more side effects and should not be used.
Intravenous amphotericin B in a liposomal formulation (trade name AmBisome) may be used but is not superior; its main use is in patients who do not tolerate standard amphotericin B.
In Africa, oral fluconazole at a rate of 200 mg daily is often used. However, this does not result in cure, because it merely suppresses the fungus and does not kill it; viable fungus can continue to be grown from cerebrospinal fluid of patients not having taken fluconazole for many months. An increased dose of 400 mg daily does not improve outcomes,[33] but prospective studies from Uganda and Malawi reported that higher doses of 1200 mg per day have more fungicidal activity.[34] The outcomes with fluconazole monotherapy have 30% worse survival than amphotericin-based therapies, in a recent systematic review.[35]
Cryptococcus neoformans is an encapsulated yeast belonging to the class Tremellomycetes and an obligate aerobe that can live in both plants and animals. Its teleomorph is a filamentous fungus, formerly referred to Filobasidiella neoformans. In its yeast state, it is often found in bird excrement. Cryptococcus neoformans can cause disease in apparently immunocompetent, as well as immunocompromised, hosts.